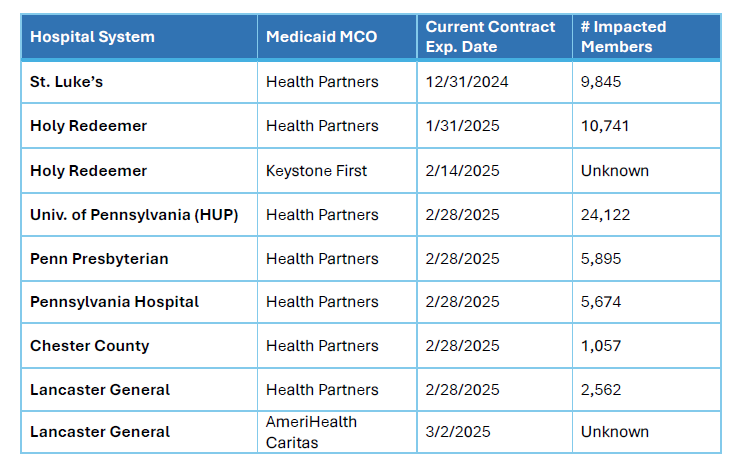
Upcoming Potential Contract Terminations Between Hospital Systems and Medicaid MCOs
Officials from the Department of Human Services (DHS) recently announced that several contracts between Medicaid Managed Care Organizations (MCOs) and hospital systems throughout the eastern part of the state are scheduled to expire at the end of this year or early 2025. The impacted hospitals and MCOs are listed in the following table:
Recall that earlier this year, the state's largest Medicaid MCO, Keystone First, and two major hospital systems in Southeastern Pennsylvania—Children’s Hospital of Philadelphia and Temple University-- took months to negotiate new Medicaid contracts, leaving patients uncertain about the future of their care. Those negotiations between Keystone First and CHOP as well as Temple extended to the eleventh hour before agreements were ultimately reached.
Medicaid MCOs are required to send letters to impacted members at least 45 days prior to a potential contract termination to ensure that the member has proper notice and time to prepare, should the negotiations for a continued contract fail. An agreement or contract extension could still be reached after the MCOs mail these member notices, as was demonstrated by the negotiations between CHOP and Temple with Keystone First earlier this year.
What Can Impacted Members Do?
People who receive notice that their doctor or hospital will no longer be in network with their Medicaid MCO have two main options: they can choose a new MCO and stay with their current hospital and/or doctors; or they can stay with their current MCO and select new doctors and other providers. Each option is discussed below.
1. Choosing a new MCO while continuing with current hospital and doctors
Medicaid enrollees who wish to remain with their current providers can switch their Medicaid MCO. All of the hospital systems mentioned in the chart above appear to be in-network with at least one other MCO as of the date of this article. This means that if that hospital's negotiations with the MCO fails, members who get care at that hospital would have at least one other MCO they could switch to in order to stay with their current hospital and doctors.
Changing MCOs can be an especially complex process for people who utilize multiple doctors or specialists, home health agencies, and/or equipment suppliers. When making the decision to change plans, people should aim to select an MCO that includes as many of these providers in its network as possible. Generally, changes to MCO enrollment must be made before the second Thursday of the month to take effect in the following calendar month.
Those who wish to change plans can compare the available MCOs, search MCO provider networks, and enroll in a new MCO by phone or online:
- Online: Visit the PA Enrollment Services website at www.EnrollNow.net
- By phone: Call PA Enrollment Services at 1-800-440-3989 (TTY: 1-800-618-4225)
2. Staying with current MCO and selecting new doctors and other providers
Just as the decision to select a new MCO is one that should not be taken lightly, choosing new doctors and other healthcare providers in order to stay with your current MCO is also a significant decision that requires careful consideration and planning.
To search providers within an MCO’s network, visit the Find a Provider tool on EnrollNow.net, or call your MCO’s Member Services Line and request a list of in-network providers. A complete directory of MCO Member Services numbers is available here, and the phone numbers can also be found on the back of individuals' MCO member ID cards.
People who are in an ongoing course of treatment and choose to remain enrolled in their MCO after a hospital contract termination can continue to see their healthcare providers for up to 60 days by requesting “continued coverage” from the MCO. The rules regarding continued coverage, also known as continuity of care, allow members to maintain access to their out-of-network doctors and other healthcare providers for a specified period of time following a change in MCOs or when their provider leaves the MCO's network. Continuity of care rights apply to services that require prior authorization as well as ongoing courses of treatments that do not need prior authorization. These rights are outlined in the state's contract with the Medicaid MCOs, known as the HealthChoices Agreement. If a member's request for continued coverage is denied, they have the right to appeal that decision.
Impacted members can request assistance in coordinating their care transitions by contacting the Special Needs Unit of their Medicaid MCO. Below are phone numbers for the Special Needs Units (SNUs) at the MCOs potentially impacted by upcoming contract terminations:
- Health Partners: 1-866-500-4571 (TTY: 877-454-8477)
- Keystone First: 1-800-573-4100 (TTY: 711)
- AmeriHealth Caritas: 1-800-684-5503 (TTY: 711)
PHLP will continue to monitor the above contract negotiations and share updates as we learn them.
