Certain Medicaid Consumers Must Select New Health Plan by August 16th
On September 1, 2022, the Medicaid physical health plans available in Pennsylvania are changing. Over 400,000 people on Medicaid will need to choose a new health plan by August 16th. The other 2.3 million people on Pennsylvania's Medicaid program will have the option to choose a new plan if they wish. In preparation for this transition, PHLP is co-hosting a virtual information session with the Pennsylvania Health Access Network (PHAN) on August 10th at 2:00 PM. This information session is open to consumers, providers, and advocates. Register for the information session here.
Between June 22 and July 7, mailings explaining the new plan choices should have gone out to all Medicaid consumers, including both those who are impacted and must change plans because their current plan is going away, and those who are not impacted but may change plans if they wish. The mailing should have contained a letter explaining the upcoming changes as well as a plan comparison chart showing the plans that will be available in the consumer's area beginning September 1. If you are on Medicaid and you did not receive this mailing, please call PHLP's Helpline at 1-800-274-3258.
What Plans Are Changing?
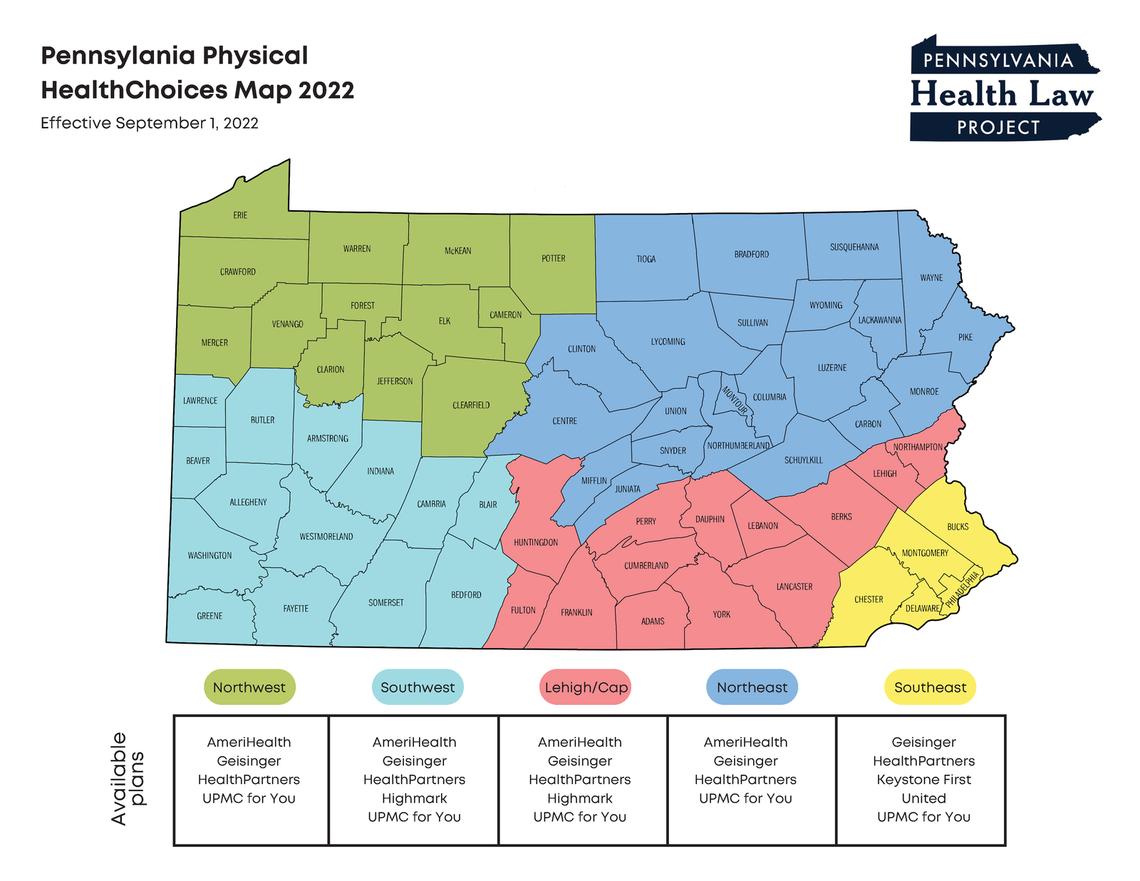
Whether your plan choices are changing depends on where you live and which plan you are in. There are several major changes:
- Aetna will no longer operate a Medicaid plan anywhere in Pennsylvania after September 1. This does not affect Aetna's CHIP Plan, which will continue to operate as it has been.
- United will no longer operate in the Southwest and Lehigh/Capital zones. This does not affect United's CHIP plan, which will continue to operate as it has been.
- Highmark (formerly Gateway) will no longer operate in the Northwest zone. This does not affect Highmark's CHIP plan, which will continue to operate as it has been.
- New plans will be available in all zones across the state. To see the plans offered in your part of the state, see PHLP’s zone-by-zone breakdown.
What Do I Need to Do?
Enrollment has begun. Consumers must change plans by August 16. Consumers who are required to change plans, and do not change, will be auto-assigned to a new plan on August 17. To compare the available plans and to make a plan change, contact PA Enrollment Services online, on their app, or by phone:
- EnrollNow.Net: Enroll in a new plan through the enrollment service website, Enroll Now. Here, individuals can compare the health plans being offered in their respective regions and make the best decision. They can also find answers to frequently asked questions.
- Mobile app: Download the PA Enrollment Services mobile app (available free of charge through the Apple store or Google play).
- Phone: Call 1-800-440-3989 (TTY: 1-800-618-4225) and select Option 6 to speak with a representative. (Open Monday through Friday, 8 a.m. to 6 p.m.).
Where Can I Get More Information?
- Register for PHLP & PHAN's Virtual Information Session on August 10th. Register here.
- The Department of Human Services (DHS) is holding virtual consumer meetings across the state. In these meetings, participants can discuss issues with enrollment and changing plans. A list of the meetings and their registration links can be found here.
- DHS has created a toolkit that discusses the plan changes and next steps for consumers. The toolkit can be found here.
- DHS has a website about the Medicaid plan changes, which is available here.
- PHLP created a factsheet to help consumers through the process of selecting a new plan. This resource gives consumers a step-by-step guide on what to consider when making their decision.
