Pennsylvania Medicaid Covers Newer Weight Loss Drugs
Medicaid consumers in Pennsylvania prescribed medication for the treatment of obesity may be able to get these medications covered if they meet certain criteria. Pennsylvania’s Medicaid program began covering the newer weight loss medications in 2023 when Wegovy was added to Medicaid’s list of preferred drugs for the treatment of obesity. Since then, Medicaid has added two other medications for weight loss to its preferred drug list: Saxenda and Zepbound.
Medicaid coverage of these weight loss drugs is available to participants who meet the prior authorization criteria (described below). Importantly, this includes people who have both Medicaid and Medicare, known as “dual eligibles”. Typically, Medicaid does not provide drug coverage for dual eligibles. Dual eligibles must get their medications covered through Medicare Part D (Medicare’s prescription drug benefit). However, Medicaid can cover certain medications excluded from the Medicare Part D benefit. Medicare Part D coverage rules specifically exclude coverage of prescription medications used solely for weight loss. Another example of excluded Part D drugs that are covered by Medicaid for dual eligibles are over-the-counter medications.
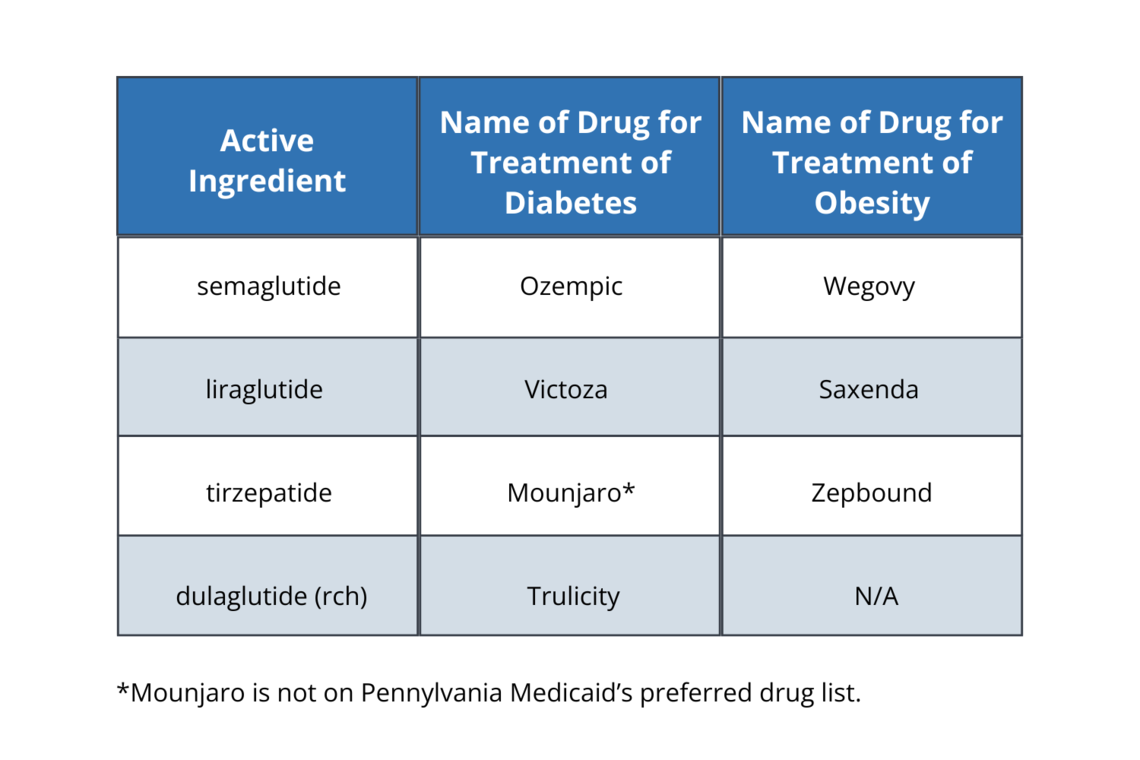
All three weight loss medications for obesity treatment are in a class of drugs (called GLP-1 receptor agonists) that have been used to treat diabetes for several years. Each of the newer weight loss drugs now on the Medicaid preferred drug list has a version of the medication used for diabetes treatment. The diabetes versions of these medications have different medication names as described below:
In order for Medicaid to cover these new weight loss drugs, a person’s doctor must submit a prior authorization request detailing that the patient meets the coverage criteria. The prior authorization guidelines are detailed in this Medicaid bulletin.
Generally, to get these drugs covered, adults over age 18 must have a body mass index (BMI) of 30 or higher (or 27 or higher with certain additional requirements), and they must have at least one weight-related health condition. Children under age 18 must have at least one weight-related health condition and their BMI must be in the 95th percentile for their age and sex based on current Centers for Disease Control and Prevention (CDC) charts.
People who have diabetes or have used a diabetes drug in the previous 120 days have an additional requirement: they must try and fail treatment on one of the preferred diabetes treatment versions of the weight loss drugs, or another preferred diabetes drug in the same drug class (GLP-1 receptor agonists).
The requirement to try and fail on one of the diabetes treatment drugs likely means people on both Medicare and Medicaid who have diabetes who are prescribed one of the above medications for obesity treatment/weight loss will need to seek coverage of a diabetes version of a weight loss drug through their Medicare Advantage Plan or Medicare Part D drug plan. Medicare plans do cover the diabetes drugs that have a weight loss version but may not cover all of these medications on their formulary (list of covered drugs). Dual eligibles who are denied coverage by Medicare or whose plan does not cover the diabetes drugs that also treats obesity may face challenges accessing the medication needed for weight loss. Those individuals are encouraged to contact PHLP for assistance.
People have a right to appeal if Medicaid denies coverage for the new weight loss drugs after a doctor submits the prior authorization showing the patient meets the criteria. Contact the Pennsylvania Health Law Project (PHLP) Helpline at 1-800-274-3258 for advice and/or assistance with appealing the Medicaid denial, or for help navigating Medicare and Medicaid coverage to access these drugs.
