Latest Updates: CHC Waiver Terminations
The PA Department of Human Services recently made changes to its process for redetermining clinical eligibility for the Community HealthChoices (CHC) waiver. They also updated policy guidance to the County Assistance Offices to clarify requirements ensuring that people keep waiver benefits if they appeal a termination action quickly. The right to keep benefits during an appeal is a critical protection under the Medicaid program when action is taken to end coverage or services that someone has been getting. As of mid-October 2023, more than 1,700 people were sent termination notices by the Office of Long-Term Living (OLTL), the office that oversees the CHC program. Several thousand more people are in the process of having their eligibility reviewed.
Background
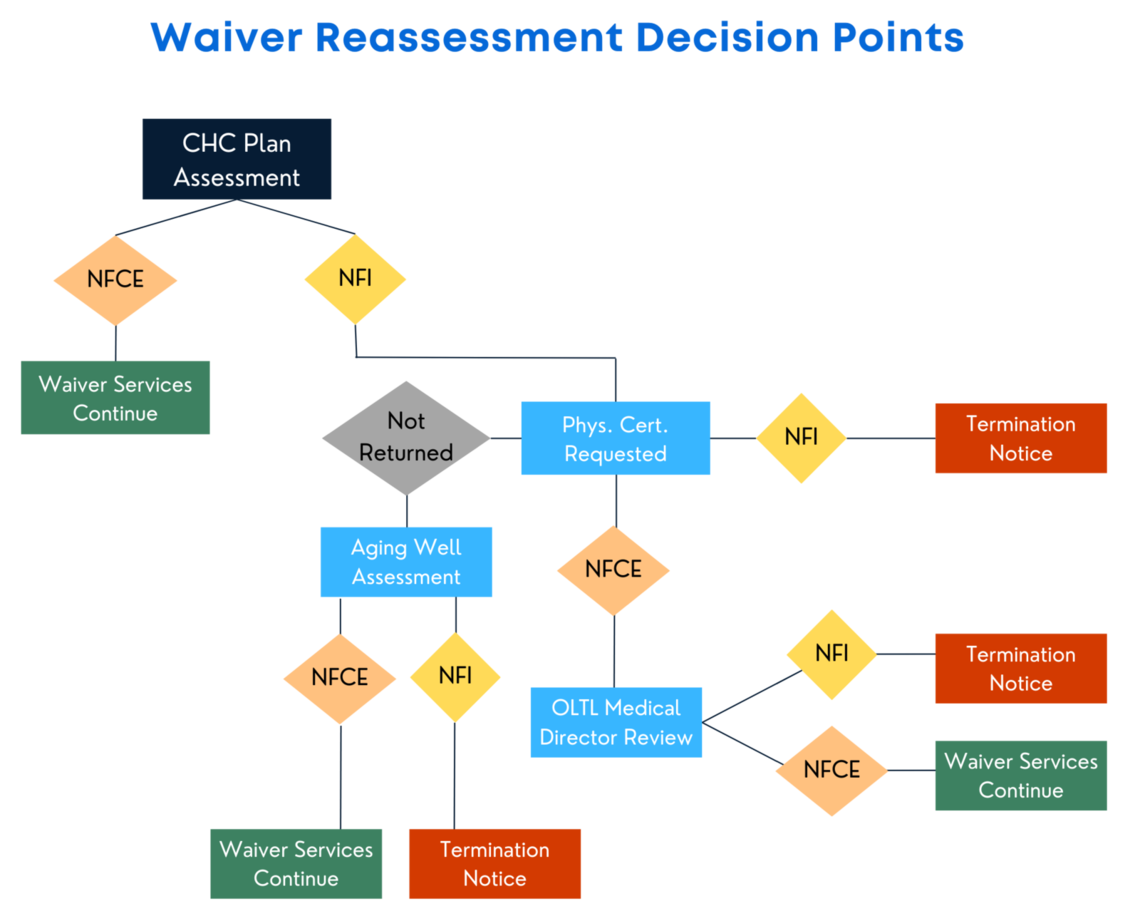
As previously reported, Pennsylvania began redetermining medical (clinical) eligibility for the CHC waiver last year. This process starts with an assessment by the person’s CHC Service Coordinator. Answers to certain questions are then used to determine whether a CHC participant continues to meet the medical (clinical) criteria needed to stay eligible for the CHC waiver. If someone is found to no longer qualify after their assessment, the CHC plan asks the participant’s doctor to complete a Physician Certification form indicating whether the doctor thinks the person meets the medical eligibility criteria.
- If the participant’s doctor agrees that the person is no longer eligible for the CHC waiver, OLTL takes action to end the CHC waiver.
- If, however, the doctor writes on the form that the person does still meet the medical eligibility criteria, the OLTL medical director reviews the case to make a final decision about whether or not the person still qualifies.
As of October 2023, OLTL’s medical director found that more than 98% of the people whose cases were reviewed no longer qualified for the CHC waiver and OLTL moved forward with ending their waiver.
Regardless of where in this process a person is found to no longer qualify, they must get written notice telling them why they no longer qualify, and this notice must be sent before the CHC waiver ends. At this time, written notices are being sent by OLTL as well as the County Assistance Offices. A person who receives either or both notices should file an appeal right away. Appeals must be sent in writing; the notices should include an appeal form to fill out and return. If someone appeals within 15 days of the mail date on their notice, they should keep their CHC waiver in place during the appeal process, which can take up to 90 days.
A Change to the Process
CHC plans are waiting for Physician Certification forms for over 4,000 people who were recently assessed and found no longer eligible for the CHC waiver. Doctors have sixty (60) days to return the Physician Certification form. Given the high number of outstanding forms, OLTL started a new process in January where Aging Well, the organization that does the initial eligibility assessments when people first apply for the CHC waiver, conducts a new, in-person reassessment when the Physician Certification form is not returned.
- If the reassessment by Aging Well finds that someone no longer medically qualifies, action will be taken to end the person’s CHC waiver enrollment, and written notices will be sent in advance, with full appeal rights, as described above.
- If Aging Well finds that someone continues to meet the medical criteria, their CHC waiver enrollment and services will continue.
Updated Policy Guidance About Individuals’ Right to Keep Benefits After a Timely Appeal
The right to appeal the decision to end someone’s CHC waiver and the right to keep benefits in place during the appeal are important safeguards aimed at preventing people from being harmed by improper terminations. Unfortunately, people impacted by these CHC waiver terminations have experienced gaps in coverage and care despite filing quick appeals. To address this problem, DHS has updated its policy guidance for a second time to clarify the right to continued benefits while an appeal is pending. The updated guidance requires the County Assistance Office to reinstate the CHC waiver within one (1) business day when an appeal is filed timely (within 15 days of the mail date on the termination notice). Again, people can appeal either the OLTL notice or the County Assistance Office notice, or both! If an appeal is filed within 15 days of the mail date on either notice, the person should keep their CHC waiver in place throughout the appeal process.
Additional Information for Impacted CHC Waiver Participants
People should appeal these terminations and should do so within the 15-day deadline to keep their waiver active while the appeal is pending. Again, appeals must be filed in writing. After an appeal is filed, people should contact Aging Well at 1-888-204-0946 or info@agingwellpa.org to ask for a copy of the assessment that found them ineligible. They should review the assessment very carefully to see if the answers in the assessment are correct. If the answers are incorrect, they should ask for a new assessment by Aging Well. In PHLP’s cases, more than 95% of clients who were terminated based on the CHC plan’s annual assessment were later found eligible for the CHC waiver after a reassessment was done by Aging Well!
People who are being terminated from the CHC waiver or who experience gaps in care or coverage following a timely appeal can seek help from their local legal aid office or from PHLP’s Helpline at 1-800-274-3258.
