Big Changes Coming to Medicare Special Enrollment Periods in 2025
Starting this year, there are significant changes to the Medicare Special Enrollment Periods (SEPs) for dual eligibles—those who receive both Medicare and Medicaid—as well as individuals eligible for Extra Help with their Part D costs. These changes affect the frequency of Medicare plan changes and the types of changes that can be made.
Special Enrollment Periods (SEPs) are designed for various situations that allow individuals to switch their Medicare health or drug plan throughout the year. Common circumstances triggering SEPs include moving, losing Medicaid coverage, or losing other prescription coverage, necessitating enrollment in Part D.
For more details about Medicare enrollment periods and the SEPs that may apply, please visit Medicare’s website here. We also encourage people with questions about Medicare plan options or those needing assistance with enrollment or changes to contact PA MEDI at 1-800-783-7067.
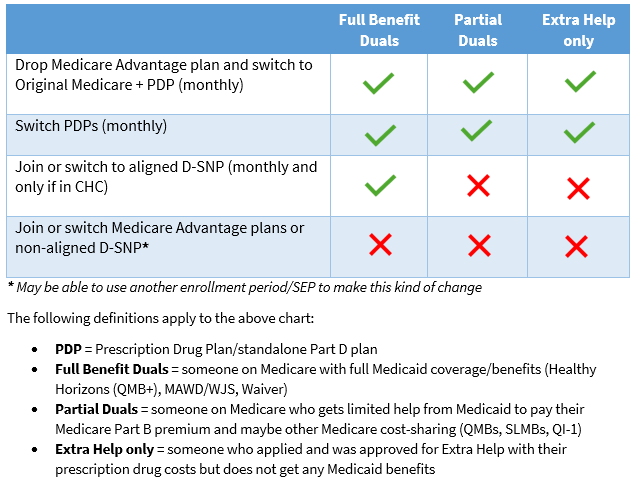
As of January 1st, the Special Enrollment Periods (SEP) for dual eligibles and people with Extra Help has shifted to a monthly schedule, with specific limitations on the types of plan changes allowed. Previously, these individuals could change their Medicare health or drug plans once per quarter during the first three quarters of the calendar year, without restrictions on the nature of those changes. Under the new guidelines, those who are dual eligible or receive Extra Help can now only make the following adjustments: 1) transition from a Medicare Advantage plan to Original Medicare and enroll in a Part D plan; or 2) switch between standalone Part D plans. Importantly, this SEP does not permit individuals in Original Medicare with a Part D plan to enroll in a Medicare Advantage plan, nor does it allow beneficiaries to switch between different Medicare Advantage plans.
Given these changes, the current Medicare Advantage Open Enrollment Period takes on even greater significance for those enrolled in Medicare Advantage plans. Beneficiaries should evaluate their Medicare Advantage plans before March 31st and utilize the Medicare Advantage Open Enrollment Period if they need to switch to a different plan for the remainder of the year.
Starting this year, a monthly "integrated care" Special Enrollment Period (SEP) has also been introduced, allowing full benefit dual eligibles to enroll in a Dual Special Needs Plan (D-SNP) that is aligned and integrated with their Medicaid managed care plan. In Pennsylvania, this new SEP is limited to dual eligibles enrolled in Community HealthChoices (CHC) for their Medicaid coverage who want to enroll into the D-SNP that is aligned with their CHC plan.
Below is a table outlining the current CHC plans and their aligned D-SNPs, which dual eligibles enrolled in CHC can use to take advantage of the new integrated care SEP.
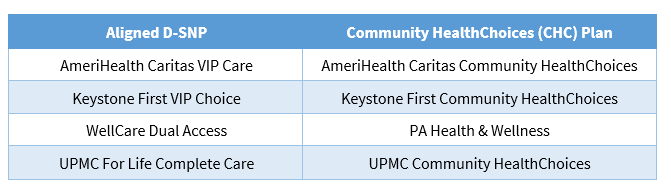
As a reminder, participants in Community HealthChoices (CHC) are not obligated to obtain their Medicare coverage through the D-SNP that is aligned with their CHC plan. Dual eligibles in CHC can choose to have their Medicare coverage through Original Medicare combined with a standalone Part D plan, or any available Medicare Advantage plan, including D-SNPs that are not aligned with their CHC plan. Additionally, it's important to note that individuals enrolled in CHC for their Medicaid coverage can change their CHC plan at any time throughout the year.